28 March 2023
Evidence of an increase in injecting drug use (IDU) at a global level highlights the need for improved coverage of interventions to prevent and manage drug-related harms among people who inject drugs (PWID), according to two new reviews led by researchers at the National Drug and Alcohol Research Centre (NDARC) and the Kirby Institute at UNSW Sydney.
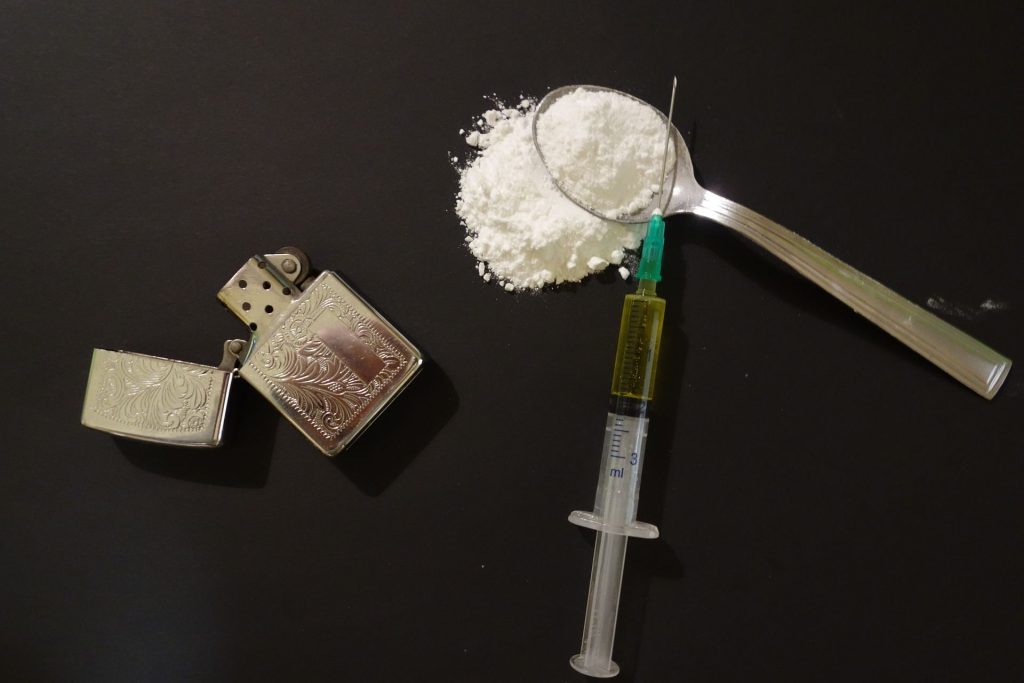
Published today in Lancet Global Health, the first review found evidence of IDU among people aged 15 to 64 years in 190 countries that comprise more than 99 per cent of the global population, an increase of 10 countries since the previous review in 2017.
This included eight countries in sub-Saharan Africa and two in the Caribbean.
Lead researcher, NDARC’s Scientia Professor Louisa Degenhardt said the landscape has changed since the last review, including increased support for research across multiple low-income and middle-income countries, shifts in patterns of drug use, the development of targets for reductions in HIV and viral hepatitis infection, and the inclusion of drug dependence treatment as one of the United Nations Sustainable Development Goals.
“Quantification of the size of the population of PWID, their demographic characteristics, and the extent of their exposure to risk behaviours and environments is essential to enable effective health policy planning,” Scientia Professor Degenhardt said.
“We had a wide focus on personal, environmental and structural risks in light of increasing recognition that a holistic view is needed to understand how to best respond to these changes.”
Professor Jason Grebely from the Kirby Institute said the review looked at the prevalence of HIV, hepatitis B virus (HBV), and hepatitis C virus (HCV) infection, the characteristics of PWID and patterns of drug use and risk history.
“Injecting drug use has now been documented in most countries and territories in the world, and HIV and HCV infection are prevalent in many populations of PWID,” Professor Grebely said.
The results show that PWID are at risk of police arrest, incarceration, sex work, and the experience of homelessness or unstable housing.
“All of these risk environments are associated with increased blood-borne virus transmission,” Scientia Professor Degenhardt said.
“There is a clear need to address the structural and environmental drivers of vulnerability, risk, and harm.”
The second review updates 2017 estimates of global coverage of needle and syringe exchange programmes (NSPs), opioid agonist treatment (OAT), and other harm reduction services that target PWID such as take-home naloxone (THN) programmes, supervised consumption facilities, and drug checking services.
It was found that 90 countries are implementing OAT (75 per cent of the PWID population) and 94 countries are implementing NSPs (88 per cent of the global PWID population).
Only five countries (two per cent of the global PWID population) are providing high coverage of both services.
Far fewer countries are implementing THN programmes, supervised consumption facilities, and drug checking services, with nine countries implementing all five services (Australia, Mexico, Canada, USA, France, Germany, Portugal, Spain, and Switzerland).
“Globally, most PWID do not have access to harm reduction services designed to reduce the public health burden and improve quality of life,” Scientia Professor Degenhardt said.
“While there has been some progress toward improved service coverage, upscaling is required to respond to the clinical and social harms that many people face.”
Epidemiology of injecting drug use, prevalence of injecting-related harm, and exposure to behavioural and environmental risks among people who inject drugs: a systematic review is being presented by Professor Jason Grebely at the Harm Reduction International Conference, HR23: Strength in solidarity in Melbourne from Sunday, 16 to Wednesday, 19 April 2023.
Epidemiology of injecting drug use, prevalence of injecting-related harm, and exposure to behavioural and environmental risks among people who inject drugs: a systematic review
The full article is available via Lancet Global Health
- Evidence of IDU was documented in 190 of 207 countries or territories that comprise more than 99 per cent of the global population aged 15–64 years.
- Globally, 14.8 million people aged 15 – 64 years are estimated to inject drugs.
- Evidence suggests that there are 2.76 million women and 12.065 million men who inject drugs globally, and that 0.4 per cent of PWID identify as transgender.
- The amount of available data on key health and social risks among people who inject drugs varied widely across countries and regions. It is estimated that 24.8 per cent of people who inject drugs globally had experienced recent homelessness or unstable housing, 58.4 per cent had a lifetime history of incarceration, and 14.9 per cent had recently engaged in sex work, with substantial geographical variation.
- Injecting and sexual risk behaviour varied considerably geographically, as did risks of harms. Globally, it is estimated that 15.2 per cent of people who inject drugs are living with HIV, 38.8 per cent have a current HCV infection, 18.5 per cent have recently overdosed, and 31.7 per cent have had a recent skin or soft tissue infection.
Global coverage of interventions to prevent and manage drug-related harms among people who inject drugs: a systematic review
The full article is available via Lancet Global Health
- Of the 195 studies included, 90 countries were found to be implementing OAT (75 per cent of the PWID population) and 94 countries implementing NSPs (88 per cent of the global PWID population).
- Five countries (two per cent of the global PWID population) are providing high coverage of both OAT and NSPs.
- Far fewer countries are implementing THN programmes, supervised consumption facilities, and drug checking services, with nine countries implementing all five services.
- Globally, it is estimated that there are 18 people accessing OAT per 100 PWID, and 35 needles and syringes being distributed per person who injects drugs per year.
Scientia Professor Louisa Degenhardt discussed the global reviews of injecting drug use on the ABC Radio National Health Report on 3 April 2023. You can listen to the full interview here.
Further information
About the NIHR Health Protection Research Unit [HPRU] in Behavioural Science and Evaluation at the University of Bristol
The NIHR HPRU in Behavioural Science and Evaluation at University of Bristol is one of 14 HPRUs across England, part of a £58.7 million investment by the NIHR to protect the health of the nation.
The NIHR HPRU in Behavioural Science and Evaluation is a partnership between the UK Health Security Agency (UKHSA) and University of Bristol, in collaboration with MRC Biostatistics Research Unit at the University of Cambridge and University of the West of England.
Each NIHR HPRU undertakes high quality research that is used by UKHSA to keep the public safe from current and emerging public health threats.
About the NIHR
The National Institute for Health and Care Research (NIHR) is the nation’s largest funder of health and care research. The NIHR:
- funds, supports and delivers high quality research that benefits the NHS, public health and social care
- engages and involves patients, carers and the public in order to improve the reach, quality and impact of research
- attracts, trains and supports the best researchers to tackle the complex health and care challenges of the future
- invests in world-class infrastructure and a skilled delivery workforce to translate discoveries into improved treatments and services
- partners with other public funders, charities and industry to maximise the value of research to patients and the economy.
The NIHR was established in 2006 to improve the health and wealth of the nation through research, and is funded by the Department of Health and Social Care. In addition to its national role, the NIHR supports applied health research for the direct and primary benefit of people in low- and middle-income countries, using UK aid from the UK government.