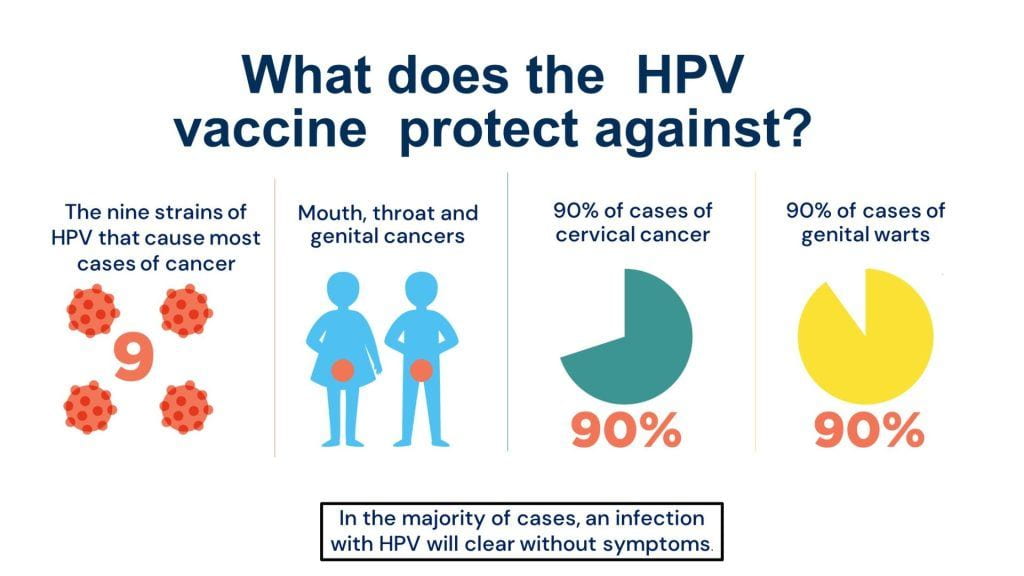
HPV is a common infection that is spread by skin-to-skin contact, including sexual contact, which can lead to the development of cancers affecting both women and men, including the cervix, vulva, vagina, penis, anus, and oral cavity.
In England, young people aged 12 to 13 years are offered immunisation against HPV as part of the NHS vaccination programme. Research has shown that in England cervical cancer has almost been eliminated among young women who were offered the HPV vaccine. The programme has also been shown to be good value for money for the NHS.
Our research has identified sustained inequalities in uptake by area and minority ethnic groups. Further, we identified unmet information needs among young people in schools where vaccination uptake is low, with implications for obtaining consent and vaccination uptake.
Addressing young people’s information needs
To address information needs among young people, we used co-production research methodologies and the ‘person-based approach’ to develop a lesson about the HPV vaccine with young people from disadvantaged backgrounds and diverse ethnic groups.
The resources for the EDUCATE lesson include films and exercises to assist learning, along with supporting the delivery of the HPV vaccination programme by providing young people with information and answering questions they may have. It prepares them to be vaccinated at school and helps them make the decision to be vaccinated or not. It is designed to be delivered before the school-based HPV vaccination session begins and can be delivered by different professionals, including teachers and immunisation nurses.
The research team partnered with the Personal, Social, Health and Economic (PSHE) Association and then resource has now been awarded their quality mark. It is available free to download from their website.
EDUCATE Video Explainer
The videos that we co-produced with young people can be found here:
‘All about HPV’
This animation provides information about HPV and the immune system.
‘Steve’s story’
Steve shares his story of developing an HPV-related throat cancer.
‘What to expect’
Young people share their experience of having the HPV vaccine in school
‘Questions and answers with an immunisation nurse’
Young people ask an immunisation questions about the HPV vaccine
‘Reassurance strategies’
Young people share some tips to help when other young people when they get the HPV vaccine.
The work was funded by the Medical Research Council’s (MRC) Public Health Intervention Development (PHIND) Programme and the Economic and Social Research Council (ESRC) Impact Acceleration Account (IAA).
Improving communication with parents
We are also carrying out a project which aims to co-design an intervention to improve parental confidence, and increase adolescent’s access to, the HPV vaccination programme. As part of this, we have developed a series of films about the HPV vaccine. The content, style and format of the COMMUNICATE films are intended to address vaccine misinformation and were informed by the preferences of vaccine hesitant, ethnically diverse parents.
The videos that we co-designed with vaccine hesitant parents can be found here:
‘Protecting my teenager from HPV’
This film provides parents with information about HPV and the HPV vaccine.
‘Penny’s story’
Penny shares her experience of having cervical cancer.
‘Safety and side-effects of the HPV vaccine’
The safety profile and the side-effects of the HPV vaccine are discussed in this film.
‘The HPV vaccine and my teenager’
Parents and healthcare professionals discuss getting teenagers vaccinated against HPV.
The films are also available in Arabic, Bengali, Polish, Somali, Urdu here.
The study was funded by the National Institute for Health and Care Research (NIHR) Research for Patient Benefit (RfPB).
Next, we plan to co-design, refine, and implement a communication strategy to support use of the films locally. We will also engage with key players nationally to share learning and explore opportunities for the films to support delivery of the HPV vaccination programme on a wider scale.
We have also been awarded BNSSG ICB Research Capability Funding to apply for funding to find out if it is feasible to carry out a large-scale study to test the effectiveness and cost-effectiveness of expansion of the HPV vaccination programme to community pharmacies to improve uptake and address inequalities.
Publications
1. Fisher H, Chantler T, Finn A, Hickman M, Letley L, Mounier-Jack S, Thomas C, & Worthington K, Yates, J, & Audrey S. Development of an educational package for the English universal human papillomavirus (HPV) vaccination programme: a co-production study with young people and key stakeholders. (2022) BMC Research Involve & Engagement. 8, 16 https://doi.org/10.1186/s40900-022-00349-7
2. Fisher H, Chantler T, Mounier-Jack S, & Audrey S. Human papillomavirus (HPV) vaccine communication tools for young people: A content analysis. Health Education Journal, April 2022. 10.1177/00178969221092135 2022.
3. Fisher H, Chantler T, Denford S, Finn A, Hickman M, Mounier-Jack S, Roderick M, Tucker L, Yates, J, Audrey S. Development of a multicomponent intervention to increase parental vaccine confidence and young people’s access to the universal HPV vaccination programme in England: protocol for a co-design study. BMJ Open. 2022
Evaluation of self-consent procedures for the schools-based Human Papillomavirus (HPV) vaccination programme

The requirement for written parental consent has been shown to be a barrier to vaccination. In England, the legal framework allows young people to be vaccinated without parental consent provided they are deemed ‘Gillick-competent’, that is, have the maturity to make their own decisions and to understand the implications of those decisions. However, an earlier study shows adolescent self-consent was not widely implemented.
New consent procedures were introduced in 2017–2018 in two local authorities in the south-west of England because of concerns about low uptake rates. The new procedures started with a request for written parental consent but also included contacting parents to ask for verbal consent, and the opportunity for adolescent self-consent if parents could not be contacted.
The study team at the University of Bristol, Sirona Care and Health, Public Health England and University Hospitals Bristol NHS Foundation Trust, undertook a mixed methods study to explore the impact on uptake and acceptability of the new consent procedures. The research was led by Drs Suzanne Audrey and Harriet Fisher from the NIHR Health Protection Research Unit in Behavioural Science and Evaluation at University of Bristol.
Project aims
The project aimed to understand how schools, parents/carers and young women respond to self-consent procedures for the HPV vaccination programme, to identify the barriers and enablers to self-consent for adolescent vaccinations.
Summary of quantitative findings
The study compared HPV vaccination uptake in intervention sites – where the new procedures were implemented – with other sites in England. Uptake in one of the local authorities increased from 76.3 per cent in 2017/18 to 82.5 per cent in 2018/19. Further analysis showed the effect was 11.5 per cent when compared with local authorities which had similar characteristics, but were not implementing the intervention, because on average their uptake decreased over the same period. But the study did not find evidence for change in uptake in the other local authority.
The study also carried out an analysis to compare uptake of the HPV vaccination programme within the intervention local authorities by ethnicity, type of school and level of deprivation. However, no evidence was found for a difference ‘before’ and ‘after’ the consent procedures were implemented.
Overall, there was some evidence that implementing the new consent procedures can improve uptake, and overcome trends for decreasing uptake, of the HPV vaccine. However, there is a need to find a way to address inequalities in uptake, which is of concern because of the disproportionate effect of HPV-related cancers among minority ethnic and more deprived groups.
Summary of qualitative findings
NIHR ARC West helped to analyse interviews with 53 participants to ask for their views about the new consent procedures. This included four healthcare professionals involved in delivering the HPV vaccination programme, eight school staff, 19 young women aged 12 to 17 years, and 22 parents.
When the study was carried out, young women were offered the HPV vaccination in Year 8, when they were between 12 and 13 years old. It was difficult for respondents to decide whether this age is the right time to self-consent because of perceived differences in the maturity of Year 8 students. One parent said: “Some 13-year olds can make really sensible decisions, and others you can’t trust them to go to the shop.”
The potential for new consent procedures to highlight the right to refuse vaccination was also a concern. One young woman said: “I don’t think we’re allowed to make the decision completely by ourselves, and I don’t think we should either because most kids will go ‘Oh, it’s a needle, I’ll go out of it, I won’t do it’ but it’s actually quite important.”
There were also concerns about the impact of self-consent on relationships within families and between professionals and the families they serve. One school staff member at an alternative education provider said: “I suppose ultimately parental relationships are really important to us… I would hate to drive a wedge in between us and the family.”
Getting consent from parents by phone was appreciated by the immunisation nurses, parents, and young women in the study. Self-consent among adolescents was rare. It’s important to understand and address the barriers to uptake outside of mainstream school-based immunisation sessions, to tackle inequalities in uptake.
Dr Suzanne Audrey, Senior Research Fellow in Public Health in Bristol Medical School, said:
“This study has highlighted unresolved issues in relation to adolescent self-consent for the HPV vaccination and potentially other vaccines and healthcare initiatives for young people. These include public and professional perceptions of young people’s rights and abilities to take responsibility for decisions affecting their health.”
The work was funded by the National Institute for Health Research (NIHR) Research for Patient Benefit Programme.
Publications
Audrey S, Evans K, Farr M, Ferrie J, Yates, J, Roderick M, & Fisher H. Implementing new consent procedures for the schools-based HPV vaccination programme: a qualitative study. British Journal of Child Health.2021. 2,2. https://www.magonlinelibrary.com/doi/abs/10.12968/chhe.2021.2.2.85
Fisher H, Evans K, Ferrie J, Yates J, Roderick M, & Audrey S. Young women’s autonomy and information needs in the schools-based HPV vaccination programme: A qualitative study. BMC Public Health 2020, 20, 10 p., 1680 https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09815-x
Audrey S, Farr M, Roderick M, Evans K., & Fisher H. How acceptable is adolescent self-consent for the HPV vaccination: qualitative findings from a process evaluation in south-west England. Vaccine 2020:38(47) https://www.sciencedirect.com/science/article/pii/S0264410X20312561
Fisher H, Hickman M, Ferrie J, Evans K, Bell M. Yates J, Roderick M, Reynolds R, Macleod J, & Audrey S, Impact of new consent procedures on uptake of the schools-based Human Papillomavirus (HPV) vaccination programme. Journal of Public Health, 2020, fdaa164, doi.org/10.1093/pubmed/fdaa164.
Fisher H, Harding S, Hickman M, Macleod J, & Audrey S. ‘Barriers and enablers to adolescent self-consent for vaccination: A mixed-methods evidence synthesis’. Vaccine, 2019: vol 37, pp. 417-4 https://www.sciencedirect.com/science/article/pii/S0264410X18316529
Audrey S, Batista Ferrer H, Ferrie J, Evans, K, Bell M, Yates J, Roderick M, Macleod J, & Hickman M. ‘The impact and acceptability of self-consent procedures for the schools-based human papillomavirus vaccine: a mixed-methods study protocol’. 2018, BMJ Open, vol 8. https://bmjopen.bmj.com/content/8/3/e021321
Batista Ferrer H, Hickman M, John Macleod, Audrey S. Adolescent self-consent for vaccinations: protocol for a mixed methods systematic review. BMJ Open, 2018: vol 8. https://bmjopen.bmj.com/content/8/5/e021335